Technology’s Role in Better Healthcare
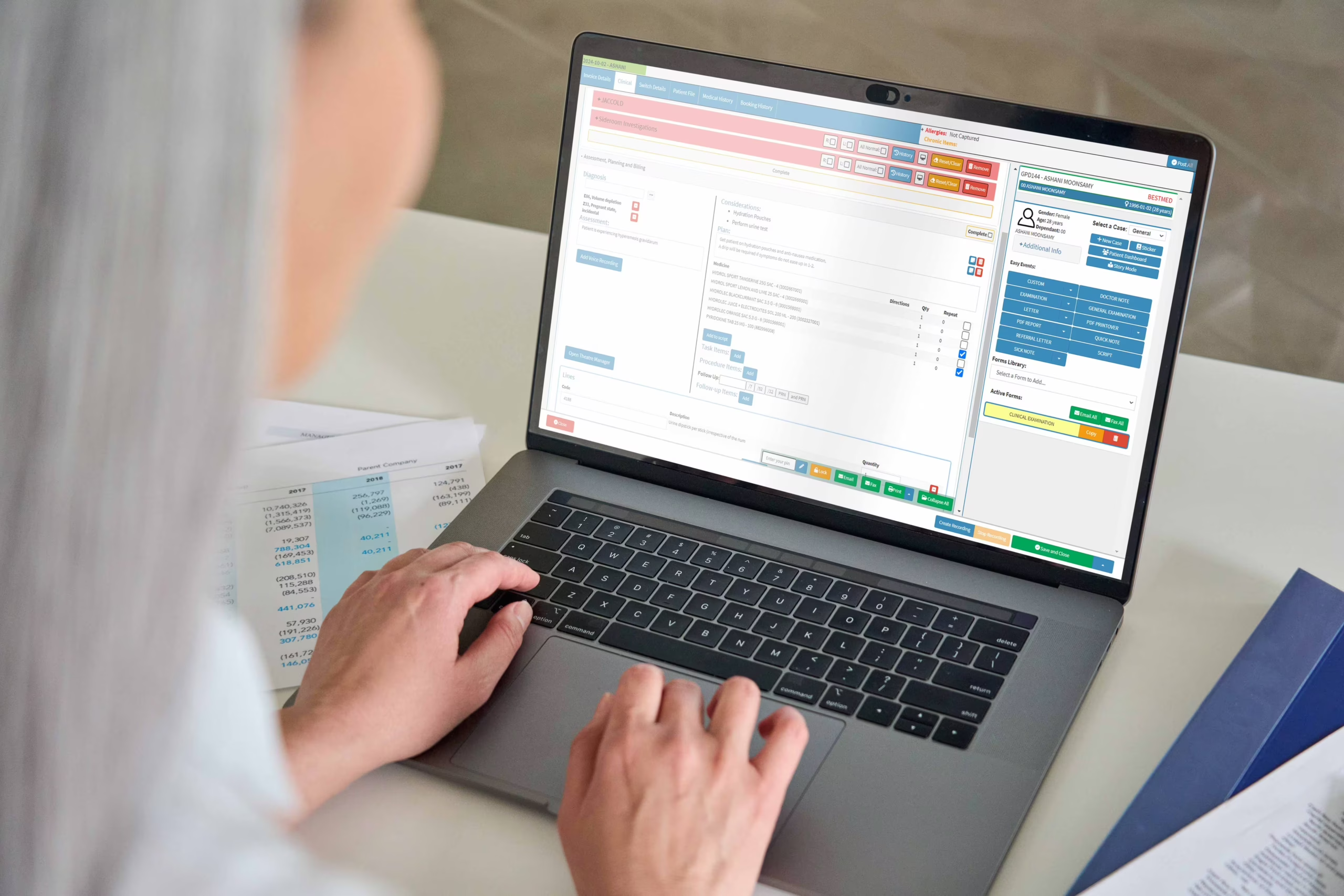
Digital tools are transforming healthcare by making everyday processes more efficient and enhancing how care is delivered. A key example of this progress is the integration of SOAP notes — a widely accepted method of clinical documentation — into practice management software. By embedding these structured notes directly into clinical systems, healthcare providers can improve workflow, strengthen team communication, and support better patient outcomes.
Let’s explore how incorporating SOAP notes into clinical software can positively impact medical practices.
1. Creating a Consistent, Efficient Documentation Workflow
Traditional patient recordkeeping, particularly on paper, can be prone to human error and inconsistency. Handwritten notes can be unclear, and manual entry consumes valuable time that could be better spent on patient care. By incorporating SOAP note templates into clinical software, practitioners can streamline documentation while ensuring every key detail is captured in an organised, repeatable format.
With predefined fields for Subjective, Objective, Assessment, and Plan sections, clinicians can quickly and easily enter relevant information. This structure promotes clarity and completeness — helping teams capture everything from presenting symptoms to diagnosis and treatment decisions. The result? Fewer errors, faster input, and better continuity of care.
2. Enabling Real-Time Collaboration Across Teams
Clear and up-to-date documentation is essential for collaborative care. Digital SOAP notes allow everyone involved in a patient’s treatment — from doctors and nurses to admin and specialists — to access the same records instantly. There’s no more waiting for physical files or scanning through disconnected notes.
When all healthcare team members can view a patient’s condition, history, and current care plan in real time, coordination becomes seamless. For example, a specialist can assess the patient’s progress without delays, while a GP can immediately act on a nurse’s observations. This immediate access leads to faster decisions and more cohesive care delivery.
3. Supporting Smarter, Safer Decision-Making
Accurate documentation is the foundation of clinical judgement. SOAP notes provide a chronological and structured way to track a patient’s progress, making it easier to spot changes, identify trends, and adjust treatment plans as needed. When integrated into a digital platform, these notes become part of a larger data set that can also support trend analysis and outcomes tracking.
Many clinical software platforms also include decision-support features that work alongside SOAP notes. These tools can alert users to drug interactions, suggest diagnostic pathways, or offer treatment guidelines based on current documentation — helping reduce errors and enhancing the quality of care.
4. Increasing Efficiency Across the Practice
Embedding SOAP notes into clinical software not only improves documentation quality but also enhances overall practice productivity. Time spent on manual data entry drops, freeing staff to focus more on care coordination and patient engagement.
Integrated systems often automate tasks like appointment reminders, prescription refills, and follow-up scheduling — all contributing to a smoother workflow. When the software also connects with billing tools, it helps ensure that procedures are accurately coded and claims submitted correctly. This reduces delays, cuts down on administrative tasks, and helps ensure steady revenue flow.
5. Meeting Compliance and Protecting Patient Data
Healthcare practices must meet strict legal standards for data privacy and security — including regulations like South Africa’s POPIA. Integrating SOAP notes into secure digital systems helps ensure that patient information is properly protected and accessed only by authorised users.
Modern clinical software typically includes encryption, audit logs, access controls, and multi-factor authentication. These features work together to minimise the risk of data breaches and help practices stay compliant with legal and ethical obligations.
The Future of Patient Care Starts with Smarter Tools
For healthcare practices aiming to enhance care delivery, reduce admin time, and maintain regulatory compliance, the integration of SOAP notes into clinical software is a powerful step forward. This structured, digital approach supports clearer documentation, better teamwork, and more informed clinical decisions.
As the healthcare industry continues to evolve, adopting advanced systems like these will be essential for maintaining high standards and meeting future demands. By embracing tools like SOAP note integration, practices can improve daily operations, reduce stress for staff, and ultimately deliver better care to every patient.
Ready to Experience the GoodX Difference?
If you’d like to discover how GoodX can make your clinical note-taking smoother and more efficient, contact us today: 📞 +64 21 234 0563 🌐 https://goodx.co.nz